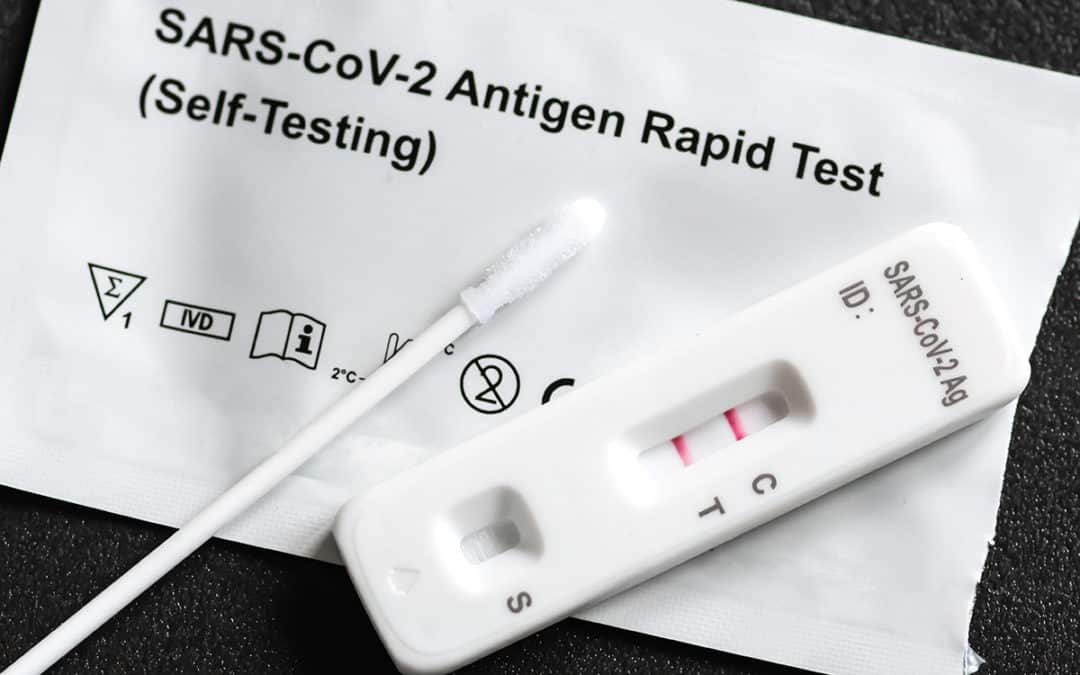
If you test positive for COVID-19, you should stay home for at least 5 days and isolate yourself from others in your home. You are likely most infectious during these first 5 days. • Wear a high-quality mask if you must be around others at home and in public. • Do not go places where you are…
read more