Learn about the nutritional benefits of artichokes, how to prepare them, and how to enjoy them. Read More: Seasonal Spotlight: Enjoy Fresh Artichokes this Spring


Learn about the nutritional benefits of artichokes, how to prepare them, and how to enjoy them. Read More: Seasonal Spotlight: Enjoy Fresh Artichokes this Spring

Resident doctors are set to host the second annual Wilderness Medicine Conference June 29th-30th at the Valle Crucis Conference Center. Read More: Resident doctors host second annual wilderness medicine conference in the High Country

Millions of individuals across the U.S. endure a common but rarely discussed condition–hemorrhoids. Notably, Dr. Trate from AppGastro points out that by the… Read More: No more suffering in silence: AppGastro offers non-invasive hemorrhoid relief

A serving of asparagus supplies vitamin A, vitamin B6, vitamin C, vitamin E, and folacin. It also contains a healthy portion of… Read More: Spring arrives, and asparagus follows

Even if you are a healthy adult, establishing a “medical home” with a primary care provider (PCP) is a responsible, proactive approach to your health. Read More: Breaking down barriers to healthcare access
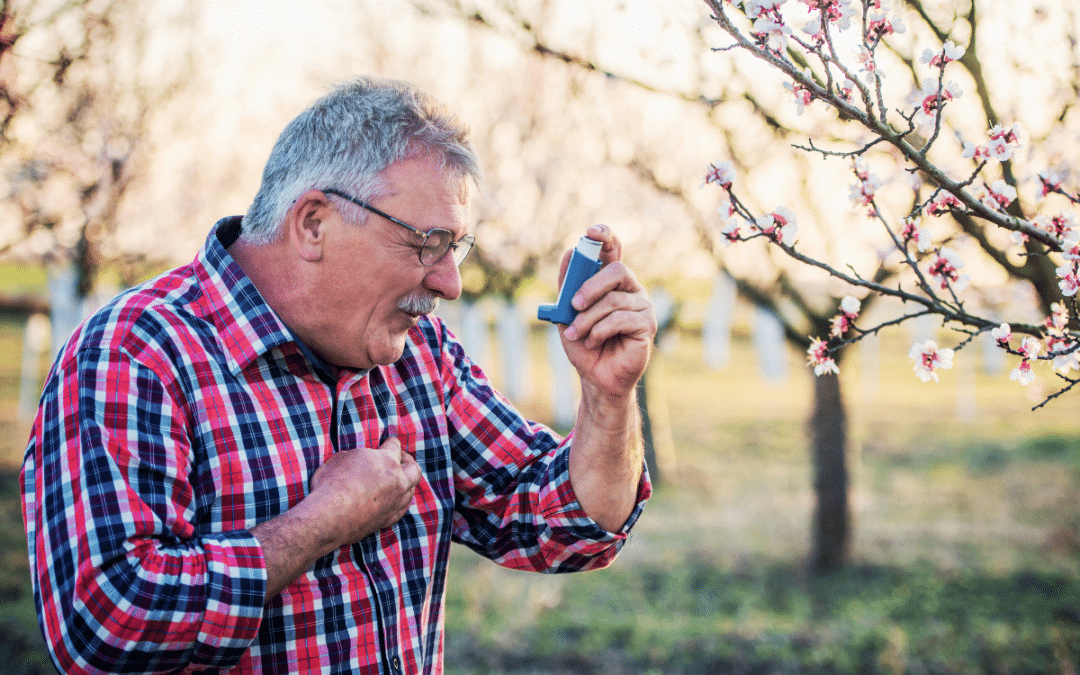
According to the Centers for Disease Control and Prevention (CDC), as of 2021, asthma affects 7.7% of the U.S. population. Asthma is a lung condition that … Read More: Clearing the Air: Exposing Asthma Misconceptions

When the weather gets cool, sweet potatoes get hot – at least for a short time. Sweet potatoes are one of those foods traditionally served at Thanksgiving, and … Read More: Sweet potatoes are good year round, not just holidays

All those unshakable New Year’s resolutions to lose weight will soon be severely tested; Valentine’s Day is coming! But could chocolate have its benefits? Read More: The surprising health benefits of chocolate: What you need to know

Do you ever feel tired in the morning or feel like you’re constantly tired throughout the day? Have you ever laid in bed at night thinking if I fall asleep right now, I’ll get 5 hours of sleep? Read More: From tossing to snoozing: The power of a sleep study

If it seems that your New Year’s resolutions are always ambushed by your inability to “stay the course,” you’ve got a lot of company. Read More: How to keep your resolutions