During a cardiac emergency, any delay in restoring blood flow increases the chance for significant damage to the heart muscle.On July 1, 2020, Watauga Medical Center (WMC) began performing cardiac ca Read More: 24/7 Cardiac Cath


During a cardiac emergency, any delay in restoring blood flow increases the chance for significant damage to the heart muscle.On July 1, 2020, Watauga Medical Center (WMC) began performing cardiac ca Read More: 24/7 Cardiac Cath

Watauga Medical Center (WMC) is embracing cutting-edge medical technology to enhance its cardiovascular care services, particularly in the treatment of calcified lesions in coronary arteries. Calcifie… Read More: New cutting-edge technology helps treat calcified lesions in coronary arteries

CCTA can be a valuable tool for maintaining your heart health. This non-invasive and quick scan can help doctors detect heart disease early and guide… Read More: Understanding CCTA: How it can benefit your heart health

In the field of healthcare, some individuals go above and beyond mere duty. They are the ones who go the extra mile to make a meaningful difference in the… Read More: Heart & soul: Kim Denny’s story of compassion & achievement

After a massive heart attack changed Tommy Smith’s weekend plans, he is grateful he was in Boone and close to Watauga Medical Center. Read More: In the right place at the right time

When dealing with chest pain, you want the best care possible – and that’s exactly what you’ll find at the Heart & Vascular Center of Watauga Medical Center. Combining state-of-the-art technology, a dedicated and compassionate team of experts, and a patient-centered approach, our Chest Pain Program has emerged as a leader in delivering exceptional cardiovascular care. Read More: Pioneering the Way in Chest Pain Care

A person dies every 34 seconds in the United States, due to heart disease. Heart disease is currently and has been the number one cause of death for too long. Read More: Do your part, to protect your heart


Virtual Tour & Photo Gallery: ARHS Heart & Vascular Center – Ashe Read More: Virtual Tour & Photo Gallery: ARHS Heart & Vascular Center – Ashe
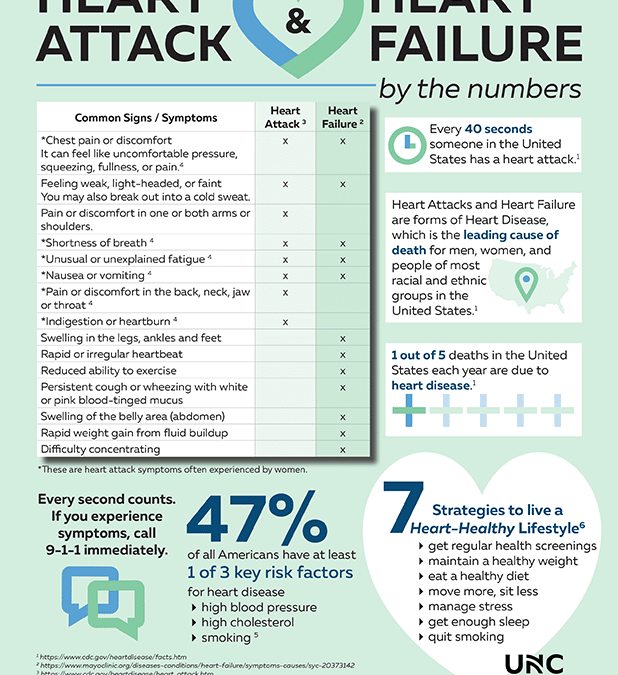
In the infographic below, you can learn about common signs and symptoms of heart failure and heart attack, risk factors, heart-healthy strategies, and facts. Read More: Heart Attack and Heart Failure: Know the Facts (Infographic)